Pneumonia Causes, Prevention and Treatment.
7 min read
Pneumonia is inflammation and fluid in your lungs caused by a bacterial, viral or fungal infection. It makes it difficult to breathe and can cause a fever and cough with yellow, green or bloody mucus. The flu, COVID-19 and pneumococcal disease are common causes of pneumonia. Treatment depends on the cause and severity of pneumonia.

Overview: Illustration comparing healthy lungs to pneumonia. Lungs with pneumonia show inflamed, fluid-filled alveoli and airways.Pneumonia causes your lung tissue to swell. It can cause fluid or pus in your lungs.
What is pneumonia?Pneumonia is an infection in your lungs caused by bacteria, viruses or fungi. Pneumonia causes your lung tissue to swell (inflammation) and can cause fluid or pus in your lungs. Bacterial pneumonia is usually more severe than viral pneumonia, which often resolves on its own.Pneumonia can affect one or both lungs. Pneumonia in both of your lungs is called bilateral or double pneumonia.What’s the difference between viral and bacterial pneumonia?
While all pneumonia is inflammation caused by an infection in your lungs, you may have different symptoms depending on whether the root cause is a virus, bacteria or fungi.
Bacterial pneumonia tends to be more common and more severe than viral pneumonia. It’s more likely to require a hospital stay. Providers treat bacterial pneumonia with antibiotics. Viral pneumonia causes flu-like symptoms and is more likely to resolve on its own. You usually don’t need specific treatment for viral pneumonia.
What are the types of pneumonia?We categorize pneumonia by which pathogen (virus, bacteria or fungi) caused it and how you got it — community-acquired, hospital-acquired or ventilator-associated pneumonia.
Community-acquired pneumonia (CAP)When you get pneumonia outside of a healthcare facility, it’s called community-acquired pneumonia. Causes include:
Bacteria: Infection with Streptococcus pneumoniae bacteria, also called pneumococcal disease, is the most common cause of CAP. Pneumococcal disease can also cause ear infections, sinus infections and meningitis. Mycoplasma pneumoniae bacteria causes atypical pneumonia, which usually has milder symptoms. Other bacteria that cause CAP include Haemophilus influenza, Chlamydia pneumoniae and Legionella (Legionnaires’ disease).
Viruses: Viruses that cause the common cold, the flu (influenza), COVID-19 and respiratory syncytial virus (RSV) can sometimes lead to pneumonia.Fungi (molds): Fungi, like Cryptococcus, Pneumocystis jirovecii and Coccidioides, are uncommon causes of pneumonia. People with compromised immune systems are most at risk of getting pneumonia from a fungus.Protozoa: Rarely, protozoa like Toxoplasma cause pneumonia.
Hospital-acquired pneumonia (HAP)You can get hospital-acquired pneumonia (HAP) while in a hospital or healthcare facility for another illness or procedure. HAP is usually more serious than community-acquired pneumonia because it’s often caused by antibiotic-resistant bacteria, like methicillin-resistant Staphylococcus aureus (MRSA). This means HAP can make you sicker and be harder to treat.
Healthcare-associated pneumonia (HCAP)
You can get HCAP while in a long-term care facility (such as a nursing home) or outpatient, extended-stay clinics. Like hospital-acquired pneumonia, it’s usually caused by antibiotic-resistant bacteria.Ventilator-associated pneumonia (VAP)
If you need to be on a respirator or breathing machine to help you breathe in the hospital (usually in the ICU), you’re at risk for ventilator-associated pneumonia (VAP). The same types of bacteria as community-acquired pneumonia, as well as the drug-resistant kinds that cause hospital-acquired pneumonia, cause VAP.
Aspiration pneumonia: Aspiration is when solid food, liquids, spit or vomit go down your trachea (windpipe) and into your lungs. If you can’t cough these up, your lungs can get infected.
Learn common symptoms of pneumonia and when you should seek medical attention.How can I tell if I have pneumonia versus the common cold or the flu?
It can be difficult to tell the difference between the symptoms of a cold, the flu and pneumonia, and only a healthcare provider can diagnose you. As pneumonia can be life-threatening, it’s important to seek medical attention for serious symptoms that could be signs of pneumonia, such as:Congestion or chest pain.Difficulty breathing.A fever of 102 degrees Fahrenheit (38.88 degrees Celsius) or higher.Coughing up yellow, green or bloody mucus or spit.Who is most at risk of getting pneumonia?You’re at an increased risk of pneumonia if you:Are over the age of 65 and or under the age of 2.
Are living with a lung or heart condition. Examples include cystic fibrosis, asthma, chronic obstructive pulmonary disease, emphysema, pulmonary fibrosis or sarcoidosis.Are living with a neurological condition that makes swallowing difficult. Conditions like dementia, Parkinson’s disease and stroke increase your risk of aspiration pneumonia.Are in the hospital or at a long-term care facility.
Have a weakened immune system. You might have a weakened immune system if you’re on chemotherapy, are an organ transplant recipient, are living with HIV/AIDS or are taking medications that suppress your immune system.
How common is pneumonia?Anyone can get pneumonia. It’s a common illness, with millions of people diagnosed each year in the United States. About 55,000 people die each year of pneumonia in the U.S. It’s the most common cause of death in developing countries.
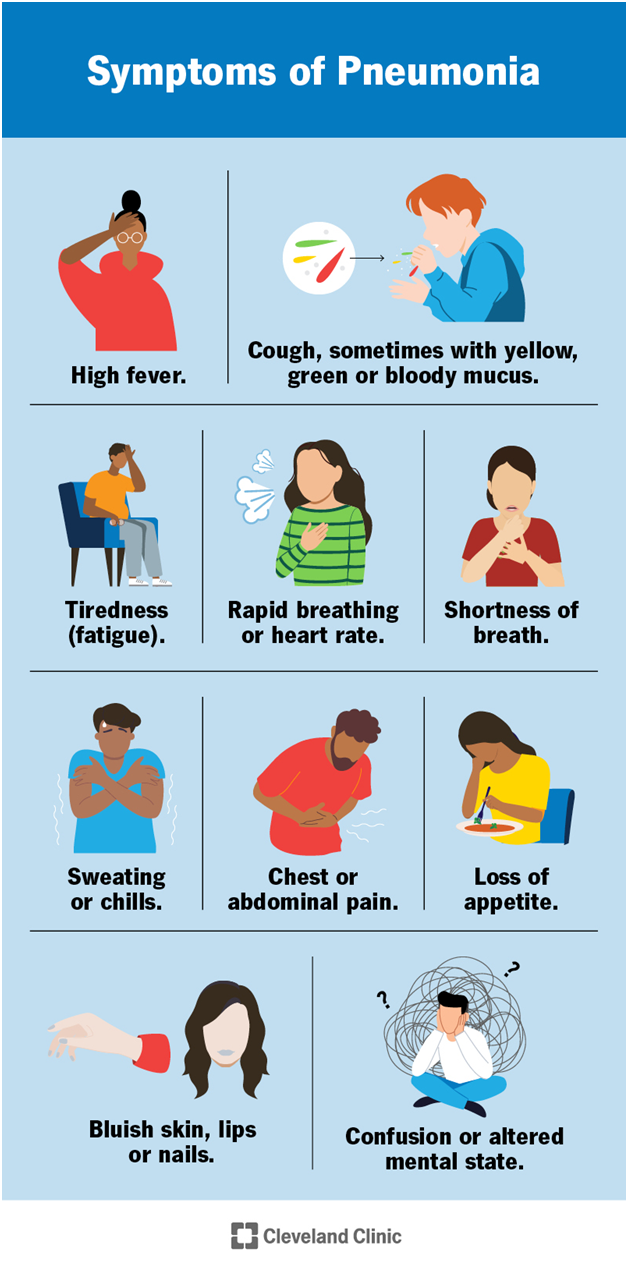
Symptoms and Causes: Symptoms of pneumonia include high fever, cough, fatigue, shortness of breath, sweating or chills, rapid heartrate and more.You won’t necessarily have all the symptoms of pneumonia. Symptoms may be different in young children and older adults.
What are the signs and symptoms of pneumonia?
Symptoms of pneumonia depend on the cause. Symptoms can range from mild to severe. Babies, young children and older adults may have different symptoms.
Symptoms of bacterial pneumonia: Symptoms of bacterial pneumonia can develop gradually or suddenly. Symptoms include:High fever (up to 105 F or 40.55 C).Cough with yellow, green or bloody mucus.Tiredness (fatigue).
Rapid breathing.Shortness of breath.Rapid heart rate.Sweating or chills.
Chest pain and/or abdominal pain, especially with coughing or deep breathing.
Loss of appetite.Bluish skin, lips or nails (cyanosis).Confusion or altered mental state.Symptoms of viral pneumonia. Symptoms of viral pneumonia usually develop over several days. You might have symptoms similar to bacterial pneumonia or you might additionally have:Dry cough.Headache.Muscle pain.Extreme tiredness or weakness.
Symptoms of pneumonia in young children: Babies and newborns may not show any symptoms of pneumonia or their symptoms may be different from adults, including:Fever, chills, general discomfort, sweating/flushed skin.Cough.Difficulty breathing or rapid breathing (tachypnea).Loss of appetite.Vomiting.Lack of energy.Restlessness or fussiness.Signs you can look for in babies and young children include:Grunting sound with breathing or noisy breathing.A decreased amount of pee or diapers that are less wet.Pale skin.Limpness.Crying more than usual.Difficulty feeding.
Symptoms of pneumonia in adults over 65: Adults over 65 or those with weakened immune systems may have mild or less noticeable symptoms of pneumonia (like cough and shortness of breath). Symptoms of ongoing health conditions may worsen. Older adults may experience:
A sudden change in mental state.Low appetite.Fatigue.What causes pneumonia?Pneumonia can develop when your immune system attacks an infection in the small sacs of your lung (alveoli). This causes your lungs to swell and leak fluids.
Many bacteria, viruses and fungi can cause the infections that lead to pneumonia. Bacteria are the most common cause in adults and viruses are the most common cause in school-aged children. Common illnesses that can lead to pneumonia include:Common cold (rhinovirus).
COVID-19 (SARS-COV-2).The flu (influenza virus).Human metapneumovirus (HMPV).Human parainfluenza virus (HPIV).Legionnaires’ disease.Mycoplasma pneumonia bacteria.Pneumococcal disease.Pneumocystis pneumonia.Respiratory syncytial virus (RSV).
Is pneumonia contagious?: Pneumonia itself isn’t actually contagious, but the bacteria and viruses that cause it are. For instance, the flu is contagious and can lead to pneumonia, but most people who get the flu won’t get pneumonia.
The bacteria that most commonly causes pneumonia, Streptococcus pneumoniae, can be spread from person to person by touching infected surfaces or through coughing and sneezing.Pneumonia caused by fungi isn’t contagious. Fungal infections aren’t spread from person to person like viruses and bacteria.
Diagnosis and Tests: How is pneumonia diagnosed?To diagnose pneumonia, a healthcare provider will ask about your health history and conduct a physical exam. They’ll listen to your lungs with a stethoscope and may perform or order additional tests. These include imaging (like chest X-rays), pulse oximetry (checking oxygen levels in your blood), blood tests or sputum (spit) tests.
Even if your healthcare provider confirms that you have pneumonia, sometimes, they can’t find the exact cause.
What tests will be done to diagnose pneumonia?Your provider may perform tests that look at your lungs for signs of infection, measure how well your lungs are working and examine blood or other body fluids to try to determine the cause of your pneumonia. These include:
Imaging: Your provider can use chest X-ray or CT scan to take pictures of your lungs to look for signs of infection.
Blood tests: Your provider can use a blood test to help determine what kind of infection is causing your pneumonia.Sputum test: You’re asked to cough and then spit into a container to collect a sample for a lab to examine. The lab will look for signs of an infection and try to determine what’s causing it.Pulse oximetry: A sensor measures the amount of oxygen in your blood to give your provider an idea of how well your lungs are working.Pleural fluid culture: Your provider uses a thin needle to take a sample of fluid from around your lungs. The sample is sent to a lab to help determine what’s causing the infection.
Arterial blood gas test: Your provider takes a blood sample from your wrist, arm or groin to measure oxygen levels in your blood to know how well your lungs are working.Bronchoscopy: In some cases, your provider may use a thin, lighted tube called a bronchoscope to look at the inside of your lungs. They may also take tissue or fluid samples to be tested in a lab.